The sacroiliac joint—or SI joint—is one of the most misunderstood areas in the body. And yet, it plays a massive role in your ability to move, feel good, and stay injury-free.
If you’ve ever looked for SI joint exercises or ways to relieve SI joint pain, chances are the info you found was generic, over-simplified, or just wrong. And that’s a problem.
A dysfunctional SI joint can prevent you from gaining strength, limit your mobility, and leave you stuck in a loop of recurring pain or injury.
Let’s fix that.
What Is the SI Joint (And Why Should You Care)?
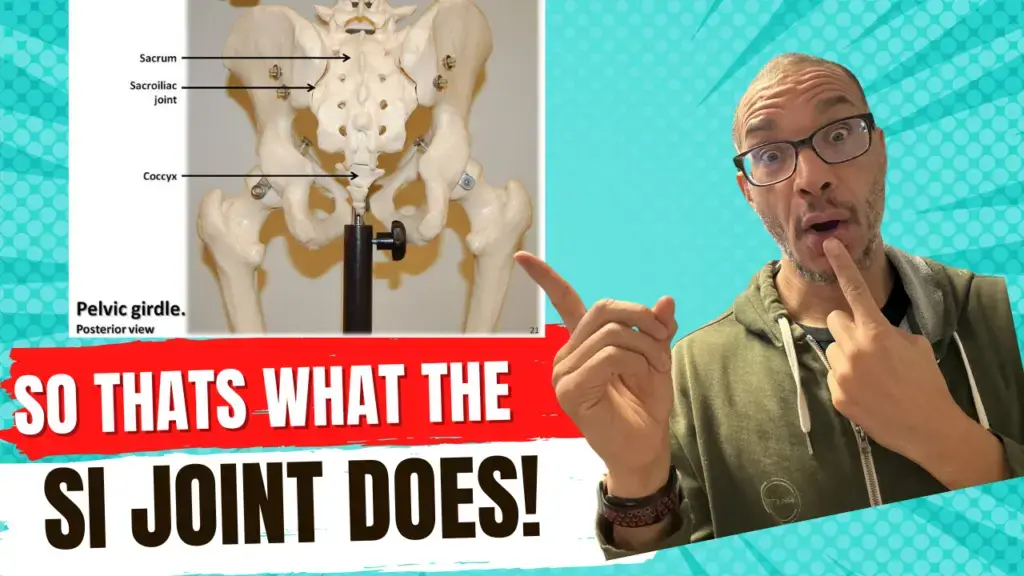
The SI joint connects your sacrum (the base of your spine) to your ilium (your pelvic bones). You have two of them—left and right—and together they form the foundation of your pelvis.
Think of your pelvis as the floor of your body. If the floor is off, everything built on top—your spine, shoulders, legs—becomes misaligned.
Here’s the kicker: SI joint issues are often asymptomatic. You might be struggling with shoulder pain, knee discomfort, or tight hip flexors—and never realize the source is pelvic instability rooted in the SI joint.
Why Standard Fixes Don’t Work
Most practitioners don’t fully understand the SI joint. Some even claim it’s not a real joint or that it doesn’t move. That’s not just wrong—it’s dangerous.
The SI joint is a total joint:
- It has a capsule
- It contains synovial fluid
- It has proprioceptors (tiny sensory “computers”)
- It’s stabilized by key muscles and ligaments
When this area is off, you don’t just lose movement—you lose the ability to communicate with your body.
A Deeper Look: Movement and Dysfunction
Physiologically, the SI joint has one primary movement axis—called the oblique axis. It helps the sacrum and ilium move together smoothly as you walk or bend.
But when dysfunction sets in, the joint can fall into 20+ different pathological movement patterns, leading to all sorts of compensations, from a false leg length discrepancy to upper-body pain.
If your treatment or exercise doesn’t account for these patterns, you’re just treating symptoms—not the cause.
My Journey With the SI Joint
I’ve been in the health and fitness field for 30 years. I started out like most trainers—using standard methods like PT and corrective exercises. But when I injured my own back (L4-L5 disc bulge with sciatic pain), those traditional approaches didn’t help.
That’s when I found osteopathy. It opened my eyes to how the body truly works: as a holistic, interconnected system.
And the SI joint? It was central to the whole picture.
How I Assess and Work With SI Joint Issues
When someone comes into my studio (or online), one of the first places I assess is the SI joint—no matter what pain they report.
Why? Because if the foundation is off, everything else will be too.
Here’s my general approach:
- Assessment – Identify which part of the SI joint is involved (lesser arm, greater arm, apex, base, etc.).
- Ligament Reboot – Using manual therapy (like TLS and pumping) to reactivate proprioceptors and restore communication.
- Fascial Work – Addressing deeper fascial chains that are often involved but ignored.
- Specific Exercise – Not just general glute or core work, but targeted movement based on what your body needs.
Muscles involved include:
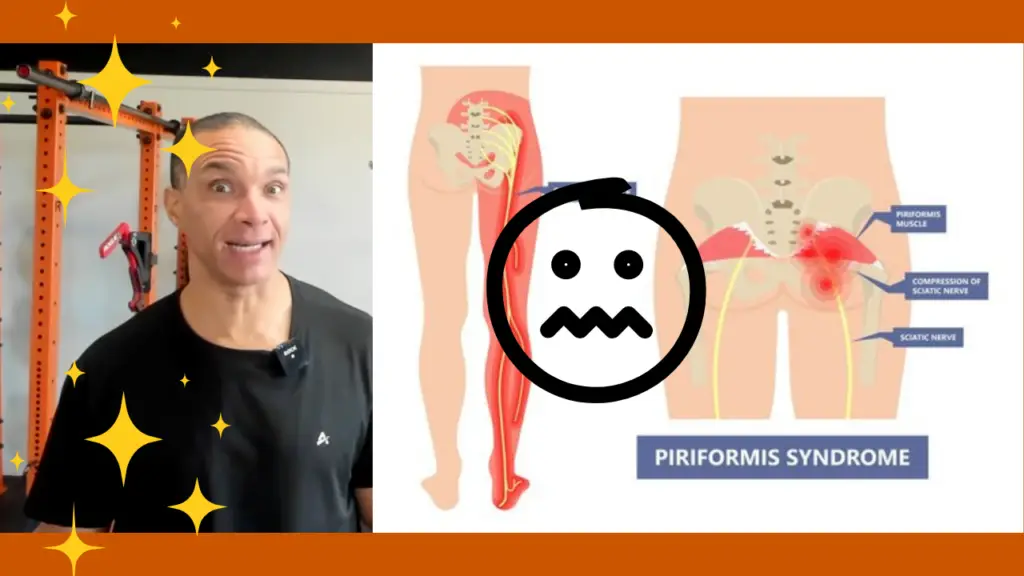
- Piriformis
- Glute Max (deep + superficial)
- Glute Med
- Obturatorius
- Iliopsoas
But again, it’s not just about muscles. It’s about chains. You have to treat the whole system.
Don’t Google “3 Moves for SI Joint Pain” (Please)
Generic exercises might help a little—or they might make things worse.
Why? Because SI joint issues are specific. The dysfunction could be from one of many regions within the joint or even a combination of them. Without proper assessment, you’re guessing.
And in the body, guessing is a great way to stay stuck.
Want to Learn More?
I share more like this every week—so subscribe, share, and join the conversation. If you’re ready to go deeper:
- 📘 Grab my free ebook: “Move Better, Reduce Pain, and Live Life On Your Terms”
- 🗓️ Book a consultation to see if we’re a good fit for private or online work
Don’t let a misunderstood joint hold back your potential. Fix the foundation—so the rest of your body can finally thrive.
it’s not just working out, it’s building a foundation for a better life.
Find out more @