When you think about independence, you might picture financial freedom or the ability to travel. But for many, independence means something much more personal: the ability to move, explore, and live life without being trapped by pain.
This is Mary’s story.
Finding Freedom from Pain
As an active person, Mary was deeply frustrated when scoliosis and SI joint issues sidelined her. The doctors told her she wasn’t a surgical candidate, and the physical therapy covered by her insurance barely scratched the surface.
Like many people, she was desperate for relief—but traditional approaches weren’t enough.
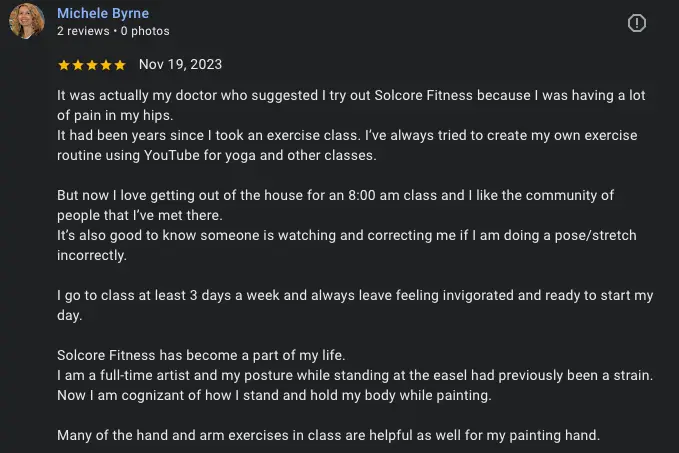
That’s when Mary found SolCore Fitness & Therapy. She was immediately drawn to our fascia-focused, holistic approach that addresses the root causes—not just the symptoms.
She joined our group classes and began private therapy sessions that worked directly with the source of her pain.
A Path to True Independence
The workouts were challenging, but never out of reach. Step by step, Mary began to rebuild her body.
Her pain decreased. Her mobility returned. Her confidence grew.
After a year and a half of committed work, Mary achieved something that once felt impossible—she completed a rugged 6-mile hike, a milestone that symbolized the independence she thought she had lost forever.
“I achieved results beyond my dreams.” — Mary
Holistic Healing That Works
Mary’s journey is a powerful reminder that when you address your body as a whole system—when you work with fascia, postural balance, and integrated movement—true independence becomes possible.
You don’t have to accept limited movement as your new normal.
You don’t have to settle for treatments that only scratch the surface.
There is a path to freedom.
👉 Watch Mary’s Full Story on YouTube
[Link to full testimonial video]
🎯 Ready to Start Your Own Journey?
If you’re ready to regain your independence and move without pain, we’d love to help.
👉 Click here to schedule your complimentary consult and see how holistic, fascia-focused training can change your life.
If you are in Santa Fe, NM or will be visiting for a stretch, come join us for our Free Community ELDOA class.
Follow the Thread—Where Movement, Fascia, and Freedom Align
Find more insight, reflection, and fascia-informed care across the platforms where we stay connected: